Healthcare Resources
Substance use and overdose are matters that touch all Philadelphians. While the Division of Substance Use Prevention and Harm Reduction (SUPHR), City agencies, and community partners work to monitor overdose trends, provide harm reduction resources, and institute policy changes to increase the health and well-being of people who use drugs in Philadelphia, we rely on clinicians to assist us in treating and educating people who use substances. Our Medical team works with clinicians, health systems and organizations, and community groups to provide the medical community with best practices, trainings, and resources to advance the care of people who use substances.
Want to learn more? Check out materials from our recent stimulant symposium, Academic Detailing Campaigns and Health Alerts, and read our recommendations below.
Xylazine and Wound Care
Treating xylazine associated wounds is a novel practice. Our Medical team convened a group of stakeholders, including physicians, surgeons, nurses, therapists, and public administrators, to conduct a thorough review of patient cases. Together, they developed a series of recommendations, and an associated webinar, for caring for people with xylazine-associated wounds.
-
SUPHR, in collaboration with the PA Department of Health and The Center for Forensic Science Research & Education (CSFRE), hosted a free virtual training for clinicians covering the best practices for treating people with xylazine-associated wounds.
To view the Caring for People with Xylazine-Associated Wounds: Training for Clinicians presentation and materials, visit the archived site and follow these instructions:
Click “login”
Click “create account”
Complete account and contact details
To proceed, click “continue”
Click “enroll”
Click “checkout”
Click “proceed”
Click “click here” under “Event Access Details” to access your training
Select training under “My Courses”
Start training video under “Virtual Platform Tutorial”
Obtain certificate after completing training video
-
SUPHR, in collaboration with the PA Department of Health and The Center for Forensic Science Research & Education (CSFRE), hosted a free virtual training for non-clinicians covering the best practices for treating people with xylazine-associated wounds.
To view the Caring for People with Xylazine-Associated Wounds: Training for Non-Clinicians presentation and materials, visit the archived site and follow these instructions:
Click “login”
Click “create account”
Complete account and contact details
To proceed, click “continue”
Click “enroll”
Click “checkout”
Click “proceed”
Click “click here” under “Event Access Details” to access your training
Select training under “My Courses”
Start training video under “Virtual Platform Tutorial”
Obtain certificate after completing training video
Treating withdrawal and initiating methadone in hospital
In response to the changing drug supply, specifically the frequent introduction of novel substances, Philadelphia hospitals are developing strategies and adapting protocols to improve withdrawal treatment for people who use drugs. Additionally, recent state and federal regulation changes are making it easier for hospitals to start patients on methadone. Thus, hospitals and emergency rooms can now do more than ever to provide excellent care to Philadelphians suffering from substance use disorder. This toolkit created by SUPHR contains scalable and effective strategies for managing withdrawal, initiating methadone in the hospital, and ensuring post-discharge continuity of care.
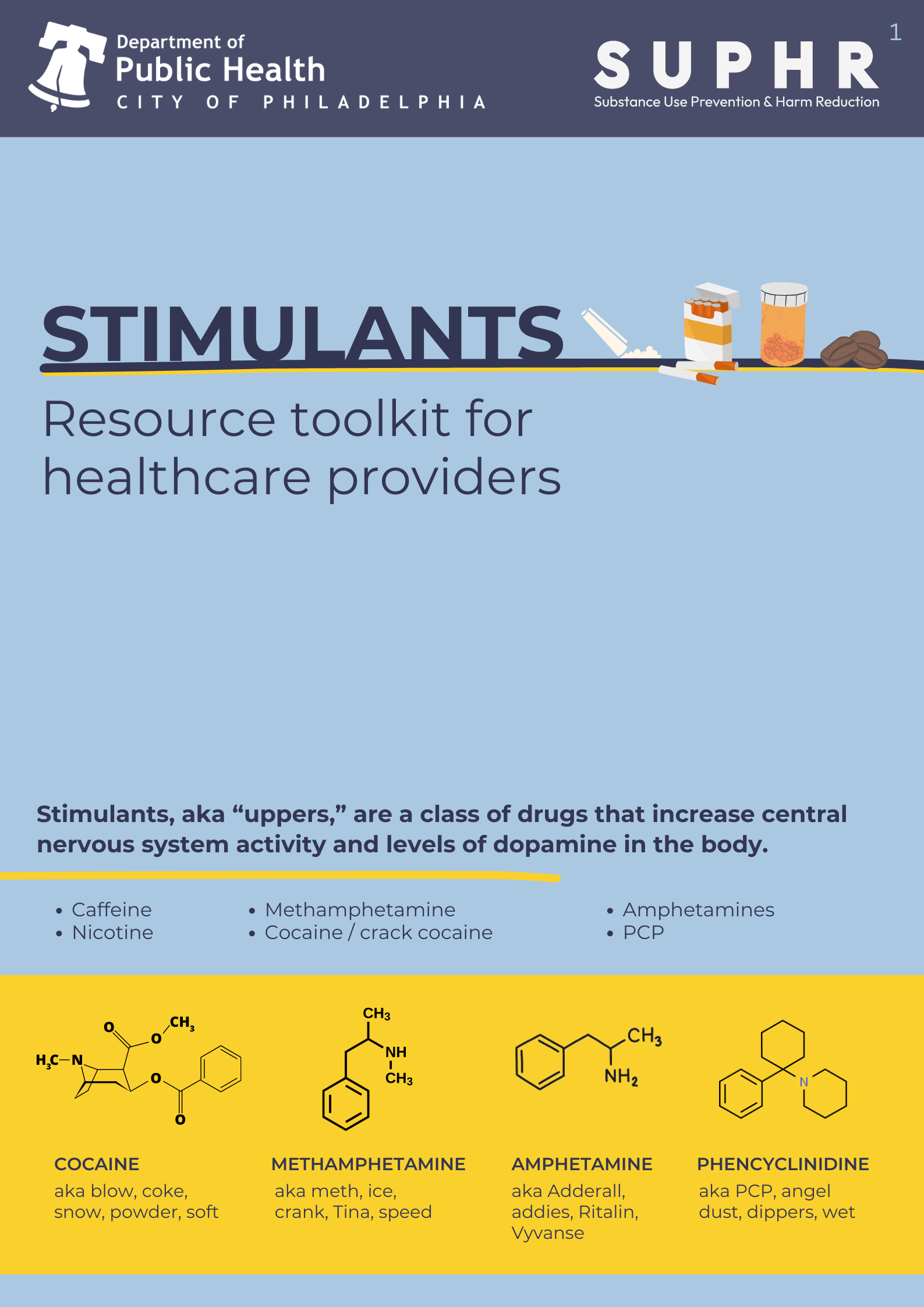
Stimulant Use Disorder
In 2023, 70% of overdose deaths in Philadelphia involved a stimulant. Despite the pervasiveness of stimulant use in the city, healthcare providers are often not equipped to address stimulant use disorder in clinical settings. In 2024, SUPHR’s Medical Team worked with the Health Federation of Philadelphia’s Substance Use Response Guidance and Education program (SURGE) to develop and curate resources for providers to better understand and address Stimulant Use Disorder in their practices.
Panelists at the 2022 Overdose Memorial Garden event Black Grief Matters
What can healthcare providers do to help Philadelphia?
Healthcare providers play a key role in addressing the impacts of the overdose crisis. As a clinician, you can get involved and help improve care for people who use drugs by getting educated on principles of harm reduction and minimizing the stigma around drug use.
Resources Created To Share
Additional Resources We Love
Local Resources:
The University of Pennsylvania’s School of Nursing manages an interactive map identifying pharmacies in Philadelphia that routinely stock and dispense buprenorphine.
Substance Use Response Guidance and Education (SURGE) offers a wide range of capacity-building services including provider collaboratives, case review sessions, and live and recorded online trainings. These trainings cover a wide range of key areas including buprenorphine in primary care practices, best practices when working with pregnant people who use drugs, and immerging topics like xylazine wound care and withdrawal management.
Jefferson Health has a collection of free, online training videos on subjects like discussing safer injections with patients and best practices for phlebotomy when working with people who use drugs.
National Resources:
Clinical Education Initiative is a New York State Department of Health AIDS Institute program that provides free, CE-accredited, online courses on harm reduction and drug user health for physicians, nurse practitioners, physician assistants, nurses, dentists, and pharmacists.
NASTAD produces resources, provides technical assistance to federal, state, and local governments and community-based harm reduction programs, and advocates for an effective science-based public health approach to address the needs of people who inject drugs.
In the Works created the eCourses and course materials they wish they had when they were running a harm reduction program. Every course is created in (paid) collaboration with people engaged in harm reduction work, including people who use drugs. A portion of the proceeds from each course goes to community collaborators and to create annual funds to distribute to organizations operating harm reduction programs in challenging environments.
National Harm Reduction Coalition builds stronger harm reduction programs through training, technical assistance, and grant-making. They also have free online resources including trainings, webinars, and eCourses.
Combat Stigma
Stigma and resulting discrimination toward people who use drugs have been linked to adverse mental and physical health outcomes including decreased treatment completion and increased syringe and equipment sharing and sexual risk-taking. People who use drugs face stigma on a number of levels: internally, interpersonally/socially, and structurally. Here are a few steps you can take as a healthcare provider to prevent the harms associated with stigma:
Interpersonal/Social
-
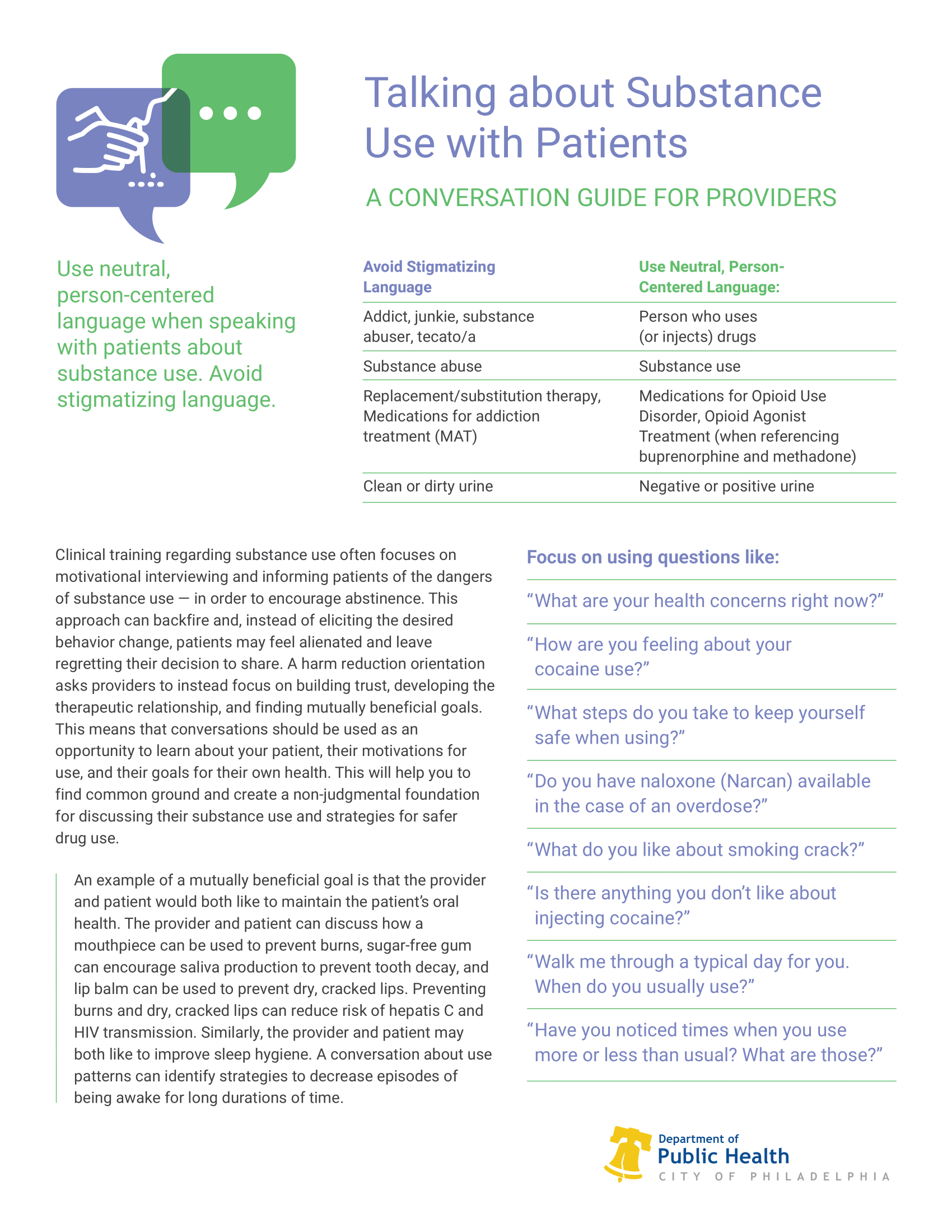
The words we use have real consequences for how people who use drugs and have substance use disorders are perceived and treated. SUPHR developed Language Matters, a language guide outlining potentially stigmatizing language and narratives and their preferred alternatives.
-
A harm reduction orientation asks providers to focus on building trust, developing the therapeutic relationship, and finding mutually beneficial goals. See this Conversation Guide for Providers to learn more about how to use conversations as an opportunity to learn about your patient, their concerns and goals for their own health, as well as their motivations for use.
-
Methadone and buprenorphine have been found to keep patients engaged in care and reduce all-cause and overdose-related mortality and injection-related morbidity, even when prescribed in interim capacities. Becoming trained to provide buprenorphine to patients increases much-needed access to this medication and helps to prevent further harms of the overdose crisis.
-
People who use drugs benefit from the support of others with a lived experience of substance use. Studies have found that the presence of Certified Peer Specialists (CPSs) in healthcare settings can decrease substance use and increase retention in treatment and, overall, assists in establishing trust between the patient and healthcare team.
-
People who use drugs deserve to be treated with dignity and respect and should be granted the same autonomy as any other patient. If you think that someone who uses drugs is facing discriminatory behavior, speak up.
Structural
-
Contact-based educational interventions (talks, trainings, and workshops facilitated by people who use drugs) with medical students, substance use counselors, and police officers have been found to increase comfort working with, and overall attitudes toward, people who use drugs.
-
Healthcare providers, especially clinicians, are trusted by the public, including lawmakers and law enforcement. Because of this influence, healthcare providers are well-positioned to advocate for the rights and dignity of people who use drugs. This can look like a few things including advocating for:
Low-barrier health and social services including same-day buprenorphine induction, mobile methadone, and walk-in primary care. For example, if a housing program requires that clients are sober to qualify for housing, one can discuss the benefits of housing on substance use outcomes and the evidence supporting housing first models used by programs like Pathways to Housing.
-
For example, if a community group is protesting to prevent a syringe service program from opening in their neighborhood, get familiar with the evidence. According to the CDC, people who inject drugs who attend an SSP regularly are more than five times as likely to enter treatment for a substance use disorder and nearly three times as likely to report reducing or discontinuing injection than those who have never been to a program. Studies have also shown benefits to community health as SSPs reduce syringe litter, HCV transmission, and even prevented an estimated 10,000 new cases of HIV among people who inject drugs in the first 10 years of their existence in Philadelphia.
-
For example, ensuring that policies dictate that urine drug screening is used as a counseling tool and that results do not result in punitive action toward clients such as removal from the program.
-
Speaking up in support of laws to prevent discrimination toward people who use drugs and for amendment and repeal of laws that criminalize people who use drugs are incredibly important. Read Structural Stigma In Law: Implications And Opportunities For Health And Health Equity for examples.
Language matters! Use our guide to help you discuss substance use and people who use drugs.
Keep Up-To-Date
SUPHR Data Dashboard
A one-stop shop for citywide data related to substance use and overdose trends. We have interactive data visualizations on acute care and hospitalizations, fatal overdoses, infectious diseases, naloxone distribution, sales, prescribing, and substance use treatment. This information can help providers understand the landscape of substance use in Philly and how trends have shifted over time.
PDPH Health Information Portal (HIP)
Philadelphia Department of Public Health maintains the HIP to communicate important health-related information to Philadelphia-area healthcare professionals. This website hosts all PDPH Health Alerts, but all alerts specific to the care of people who use drugs can also be found on our website.
In 2022, increasing amounts of the veterinary tranquilizer xylazine were identified in the Philadelphia illicit drug supply. SUPHR published two alerts to equip providers with the most up-to-date information to meet the evolving needs of people who use drugs, including intensified wound care needs and tandem opioid-xylazine withdrawal management. Previous publications have alerted healthcare professionals to spikes in HIV and hepatitis A cases among people who use drugs, the increasing prevalence of fentanyl overdoses associated with counterfeit pills, and the closure of suboxone practices in Philadelphia.